In recent years, home pulse oximeters have become increasingly popular, especially among individuals monitoring respiratory conditions like COPD or COVID-19. While these devices offer convenience, many users fall prey to misconceptions that can lead to improper usage or misinterpretation of results. Understanding these pitfalls is crucial for accurate health monitoring.
One widespread misunderstanding is that all home pulse oximeters provide medical-grade accuracy. While FDA-approved devices undergo rigorous testing, not all commercially available models meet these standards. Factors like skin pigmentation, nail polish, or poor circulation can significantly affect readings. Users often don't realize that environmental conditions such as bright ambient light or movement during measurement can also skew results. The assumption that a single reading provides a complete picture of oxygen saturation levels is particularly dangerous, as trends over time typically offer more valuable clinical information.
Another area of confusion involves the interpretation of normal ranges. Many people believe that any reading above 90% is automatically safe, ignoring the importance of baseline measurements. What constitutes a normal reading can vary between individuals based on their overall health status. For someone whose typical oxygen saturation is 98%, a drop to 92% might signal a problem, while another person might normally sit at 94%. The context of the reading matters just as much as the number itself.
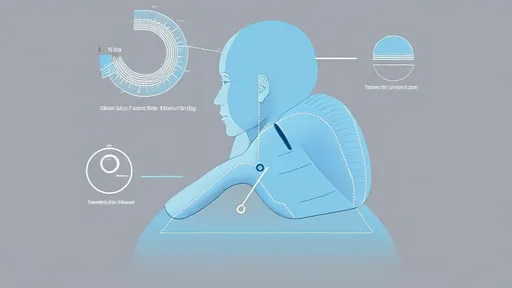
Proper device placement frequently gets overlooked in home settings. Clinical staff receive training on optimal finger positioning and monitoring duration, but home users often rush the process. The oximeter needs time to stabilize—typically about 30 seconds to a minute—to provide an accurate reading. Many users make the mistake of moving their hand or removing the device too quickly. Cold fingers can also impair detection, yet few think to warm their hands before taking a measurement.
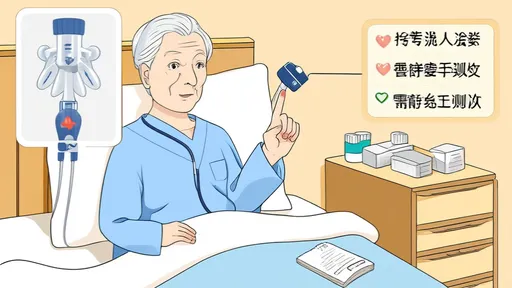
Perhaps the most dangerous misconception is treating oximeter readings as a substitute for professional medical assessment. While these devices serve as helpful screening tools, they cannot replace comprehensive evaluation by healthcare providers. Symptoms like shortness of breath, confusion, or chest pain should never be ignored simply because the oximeter shows normal numbers. The limitations of home devices become particularly apparent in cases of carbon monoxide poisoning, where oxygen saturation may appear normal despite life-threatening oxygen deprivation at the cellular level.
Maintenance and calibration represent another blind spot for many home users. Unlike hospital equipment that undergoes regular servicing, personal oximeters often get used for years without checks. Battery strength diminishes over time, potentially affecting performance. The sensors and LEDs that form the heart of these devices can degrade with prolonged use. Most manufacturers recommend periodic accuracy verification, yet few consumers follow these guidelines.
The timing of measurements introduces further potential for error. Oxygen saturation naturally fluctuates throughout the day and varies with activity levels. Taking readings immediately after exercise or while lying in certain positions may not reflect typical values. For patients with sleep apnea, nighttime readings often prove most valuable, yet many focus solely on daytime measurements. Understanding these physiological variations helps create a more complete picture of respiratory health.
As home health monitoring becomes more prevalent, education about proper oximeter use grows increasingly important. These devices offer valuable insights when used correctly, but blind trust in their readings can lead to false reassurance or unnecessary alarm. Combining oximeter data with symptom tracking and professional guidance provides the most effective approach to respiratory health management. Users who recognize the limitations of home monitoring while appreciating its benefits position themselves to make truly informed health decisions.

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025
By /Jul 28, 2025

By /Jul 28, 2025
By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025
By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025

By /Jul 28, 2025
By /Jul 28, 2025